The
most common complication was retro-prosthetic membrane (RPM) formation which
occurred in 6 eyes. One eye developed endophthalmitis and became NoPL (No
perception of light). Sterile keratolysis occurred in all 3 eyes with SJS,
which led to extrusion of the implant in 2 eyes and ultimately the eyes became
phthisic. The third eye with SJS also became phthisic. One eye with BBI
developed localized retinal detachment. All complications with their relation
to primary ocular disease are shown in Table 3.
DISCUSSION
All the nine cases
included in our study were hopeless cases with preoperative visual acuity of PL
(Perception of light) only. Three eyes had bomb blast injuries (BBI) and had
undergone corneo-scleral repairs. Three other cases were of Steven Johnson
Syndrome (SJS), with severe dry eyes (Fig. 1). All the nine eyes had severely
vascularized and totally opaque corneae.
Out of the three
cases of BBI, only two retained navigational vision (finger counting close to
eye) till last follow up visit. One of these two had posterior pole preretinal
fibrosis and other one had localized retinal detachment. Third patient
developed corneal melting followed by endophthalmitis and extrusion of the
implant. We could not find any study in literature pertaining to the use of
Boston KPro in eyes with BBI. However, Harissic- Dagher and Dohlman in their
paper “The Boston keratoprosthesis in severe ocular trauma” mentioned 6 cases
of mechanical trauma out of their total 30 studied cases. In their research
anatomic success was achieved in 5 out of 6 mechanically traumatized eyes6.

Fig. 1: Severe dry ocular surface in Steven Johnson Syndrome.
Three eyes with SJS
also had poor outcome (Fig. 2).
One eye retained 20/200 vision in first year but after
that the cornea started melting and the KPro extruded. Other eye of the same
patient became phthisic within two months of the KPro implantation and vision
did not improve from PL. Third patient

Fig. 2:
Boston KPro in Steven Johnson Syndrome.
initially obtained 20/60
vision after one week of surgery but after that it started deteriorating and
cornea started melting. Within a month the KPro extruded and eye became
phthisic. These three eyes had severe dry ocular surface and it is this dryness
that determines the retention rate of the device. According to a study from
Massachusetts eye and ear infirmary by Yaghouti F and colleagues, the outcome of KPro surgery is worse in patients with SJS7.
In this condition chronic inflammation around the KPro makes the tissue
vulnerable to necrosis, melting, leakage and infection. In this study7it
is demonstrated that 33% of eyes with SJS maintained 6/60 (20/200) vision for 2
years. This figure was minimal as compared to chemical burns (64%), ocular
cicatricial pemphegoid (72%) and non cicatricial causes (83%). Another study
from same institute mentions the use of corticosteroids (even in low doses) in
SJS causes tissue melt and perforation8. In contrast, in a study by
Sayegle RR et al on fifteen patients with SJS, there was no KPro extrusion or
endophthalmitis9. In this study only six eyes underwent type-1 KPro
while the rest underwent type-2 KPro implantation.
Two of our cases were
of healed corneal ulcer with corneal vascularization. Both of these had
undergone penetrating keratoplasty once, but failed. Both of them retained the
KPro till last follow up. Visual acuity improved to 10/200 and 20/200 after 3 months but reduced again
at last follow up. One patient developed retro-prosthetic membrane and other
developed glaucomatous optic atrophy. Both these complications are known
complications in eyes with type 1KPro.
One of the patient in
this series was a 12 years old girl with Peter anomaly. She had nystagmus since
early childhood. In initial postoperative period, there was no improvement in
vision but after 4 months she had developed navigational vision and the KPro
was retained. Use of Boston KPro is gaining popularity in pediatric population.
According to a study by Aquavella JV and colleagues the Boston KPro establishes
and maintains a clear pathway and does not prejudice the management of glaucoma
or retinopathy in children10.
COMPLICATIONS
Most common
complication in our cases was retroprosthetic membrane (RPM) formation in
6(66.6%) cases. These membranes were thick and vascularized. Only in two cases
membranectomy was possible with Nd-Yag laser, while in other four cases the
membrane was too thick to respond to Nd-Yag laser. In a study by Shihadeh and
Mohidat on 20 eyes, the frequency of RMP formation was 45% and all of them
treated successfully with Nd-Yag laser11. Its frequency is 43% in a
study by Bradley et al12, 25% in a multicentre study by Zerbe et al13
while 27% - 35% in prior published data7. According to one
hypothesis RPM formation may be caused by inflammatory cells reacting to
polymethyl methacrylate material of KPro14. Another theory about RPM
formation is mentioned by Colby, [15] according to which the
histopathological fibrous structure of RPM originates from host stromal cells
that migrate through gaps in the graft host tissue junction. In our study
highest rate of RPM could be due to excessive inflammation in cases with SJS and
BBI.
Glaucoma is another
common and the most important vision threatening complication after Boston KPro
implant16. One patient (11.1%) of our series developed glaucoma
after surgery. This patient disappeared and reappeared after about 8 months
with glaucomatous optic atrophy and high IOP detected digitally. In many
studies glaucoma has been mentioned as a postoperative complication with
different frequencies. Zerbe et al mentioned 15 % of their cases had high IOP
after surgery13. Shihadeh et al mentioned it in 25% eyes11,
and Chew et al indicated in 35% eyes14. In addition many patients
have preexisting glaucoma. Previous studies from multiple institutes have
mentioned prevalence between 36 and 76%13,14,17-19. This is because
eyes that need Boston KPro have undergone multiple anterior segment surgeries
or have diseases that cause intraocular inflammation and need to use steroid20.
“Steroids response ocular hypertension” is prevalent among these patients which
can contribute to development of glaucoma21. Glaucoma drainage
devices are the mainstay for long term control of glaucoma but these have their
own complications which can cause significant visual loss22.
Endophthalmitis is
another damaging complication following Boston KPro implantation. One case of
our series developed severe endophthalmitis two months after KPro implantation
and that led to extrusion of the implant and loss of vision to NoPL (no
perception of light). This was an eye with BBI and did not respond to
intravitreal vancomycin. Robert and colleagues reviewed endophthalmitis
following Boston KPro in literature from 2001 to 2011 and found that its
prevalence was 5.4% and gram positive bacteria are the most common agents
responsible23. Rarely fungal endothalmitis can also occur and its
rate is higher in patients using vancomycin prophylaxis and patients wearing
therapeutic contact lens24.
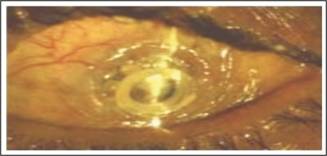
Fig. 3:
Sterile Keratolysis in eye with Boston KPro.
Three (33%) implants
of our case series were extruded. Causes of extrusion were endothalmitis in one
case and sterile keratolysis (Fig.3) in 2 cases of SJ syndrome. In a study by
Ciolino and colleagues on 300 eyes where Boston KPro type 1 was implanted,
21(7%) eyes failed to retain the device25. In this study causes of
extrusion include sterile keratolysis, infection and dense RPM. A high figure
of 33% extrusion in our series is due to selection of high risk cases for KPro
implant i.e., SJ syndrome and BBI.
CONCLUSION
Type 1 Boston
Keratoprosthesis implant still has poor prognosis in patients with SJS and
severely traumatized eye like bomb blast injuries and this is mainly due to the
preexisting bad eye condition.
Author’s
Affiliation
Prof. Dr.
Ibrar Hussain
Department of Ophthalmology,
Khyber teaching hospital, Peshawar, Pakistan.
Role of
Author
Prof.
Ibrar Hussain
Study
design, data collection, result compilation, references collection and article
writing.
REFERENCES
1.
John PW, Srinivasan M, Madan PU. Corneal blindness: a global perspective. Bull World Health Organ,
2001; 79: 214-221.
2.
Pellier de Quengsy G.
Precis au cours d’ operations sur la chirurgie des yeux. Paris: Didot, 1789.
3.
Barber JC.
Keratoprosthesis: past and present. Int Ophthalmol Clin. 1988; 28: 103-9.
4.
Hicks CR, Fitton JH, Chirila TV, Crawford GJ, Constable IJ. Keratoprosthesis: advancing toward a true artificial cornea. Surv
Ophthalmol. 1997; 42: 175-89.
5.
Dohlman CH, Schneider H, Doane MG. Prosthokeratoplasty. Am J ophthalmol. 1974; 77: 694-700.
6.
Harissi – Daghaer M, Dohlman CH. The Boston Keratoprosthesis in severe ocular trauma. Can J Ophthalmol.
2008, 43: 165-169.
7.
Yaghouti F, Nouri M, Abad JC, Power WJ, Doane MG, Dohlman CH. Keratoprosthesis: Preoperative Prognostic Categories. Cornea,
2001; 20: 19-23.
8.
Dohlman JG, Foster CS and Dohlman CH. Boston Keratoprosthesis in Steven-Johnson Syndrome: A case of
using infliximab to prevent tissue necrosis. Digital journal of ophthalmology,
2009: 15.
9.
Sayegh RR, Ang LPK, Foster CS, Dohlman CH. The Boston Keratoprosthesis in Steven – Johnson Syndrome. Invest
Ophthalmol Vis Sci. 2010; 51: 857-863.
10.
Aquavella JV, Gearinger MD, Akpek EK, McCormick GJ. Pediatic keratoprosthesis. Ophthalmology, 2007; 114: 989-94.
11.
Shihadeh WA, Mohidat HM. Outcomes of the Boston Keratoprosthesis in Jordan. Middle East
Afr J Ophthalmol. 2012; 19: 97-100.
12.
Bradley JC, Hernandez EG, Schwab IR, Mannis MJ. Boston type 1 keratoprosthesis: The University of California
Davis Experience. Cornea, 2009; 28: 321-7.
13.
Zerbe BL, Belin MW, Ciolino JB. Result from the Multicenter Boston Type 1 Keratoprosthesis Study.
Ophthalmology, 2006; 113: 1779-85.
14.
Chew HF, Ayres BD, Hammersmith KM, Rapuano CJ, Laibson PR, Myers
JS et al. Boston keratoprosthesis
outcomes and complications. Cornea, 2009; 28: 989-96.
15.
K Colby.
Boston keratoprosthesis in 2012: Preventing complication and optimizing
outcomes. Acta Ophthalmologica 2012; 90: 0.
16.
Vora GK, Colby KA.
Management of Glaucoma Following Boston Keratoprosthesis. European Ophthalmic
Review, 2012; 6: 214-7.
17.
Ma JJ, Graney JM, Dohlman CH. Repeat penetrating keratoplasty versus the Boston
Keratoprosthesis in graft failure. Int Ophthalmol Clin. 2005; 45: 49-59.
18.
Netland PA, Terada H, Dohlman CH. Glaucoma associated with keratoprosthesis. Ophthalmology, 1998; 105:
751-7.
19.
Greiner MA, Li JY and Mannis MJ. Longer-term vision outcomes and complications with the Boston
type 1 Keratoprosthesis and the University of California, Davis, Ophthalmology,
2011; 118: 1543-50.
20.
Khan BF, Harissi DM, Khan DM, Dohlman CH. Advances in Boston keratoprosthesis: enhancing retention and
prevention of infection and inflammation, Int Ophthalmol Clin. 2007; 47: 61-71.
21.
Banitt M.
Evaluation and management of glaucoma after keratoprosthesis, Curr Opin
Ophthalmol. 2011; 22: 133-6.
22.
Li JY, Greiner MA, James D, Brandt, Lim MC, Mannis MJ. Long-term Complications Associated with Glaucoma Drainage Devices
and Boston Keratoprosthesis. Am J Ophthalmol. 2011; 152: 204-218.
23.
Robert MC, Moussally K, Harissi Dagher M. Review of endothalmitis following Boston keratoprosthesis type 1.
Br J Ophthalmol. 2012; 96: 776-780.
24.
Barnes SD; Dohlman CH and Durand ML. Fungal Colonization and infection in Boston Keratoprosthesis.
Cornea, 2007; 26: 9-15.
25.
Ciolino JB, Belin MW, Todani A, Al-Arfaj K, Rudnisky CJ. Retention of the Boston Keratoprosthesis Type 1: Multicenter
Study Results. Ophthalmology, 2013; 20: 1195-1200.